A new form of mammograms, called 3D Mammography could substitute the old, painful method in a few years. The digital breast tomosynthesis takes a more detailed set of pictures than the old mammogram, making it more reliable.
Women have been advised to start getting mammograms at the age of forty. Nonetheless, a new series of recommendations from the American Cancer Society stated it is better to wait until the age of 50. According to experts, most of the time something “suspicious” will appear after a mammogram, but after more check-ups are done, turns out it was a false alarm. Additionally, other women might be asked to do a needle biopsy, where nothing was found.

Women are exposed to low-dose radiation every time they get a mammogram, which according to the American Cancer Society is the same radiation a woman would normally experience over the course of seven weeks.
Finally, mammography leads to many cases of “overdiagnosis,” in which, after the cancer found in the screening is treated, physicians determine it would have never been life-threatening. These cases generate anxiety among patients, along with physicals unnecessary interventions.
3d mammography has come to stay
Standard mammograms are not pleasant. During the procedure, the woman’s breast are tightly pressed between two metallic plates that emit low-dose radiation. 3D Mammography would become a crucial asset since it is more efficient than the old method and is virtually pain-free.
In 2014, scientists concluded that 3D mammography was up to forty percent more efficient in finding tumors than standard digital mammograms. The new screening process also diminished fifteen percent the number of misdiagnoses that lead to follow-up tests.
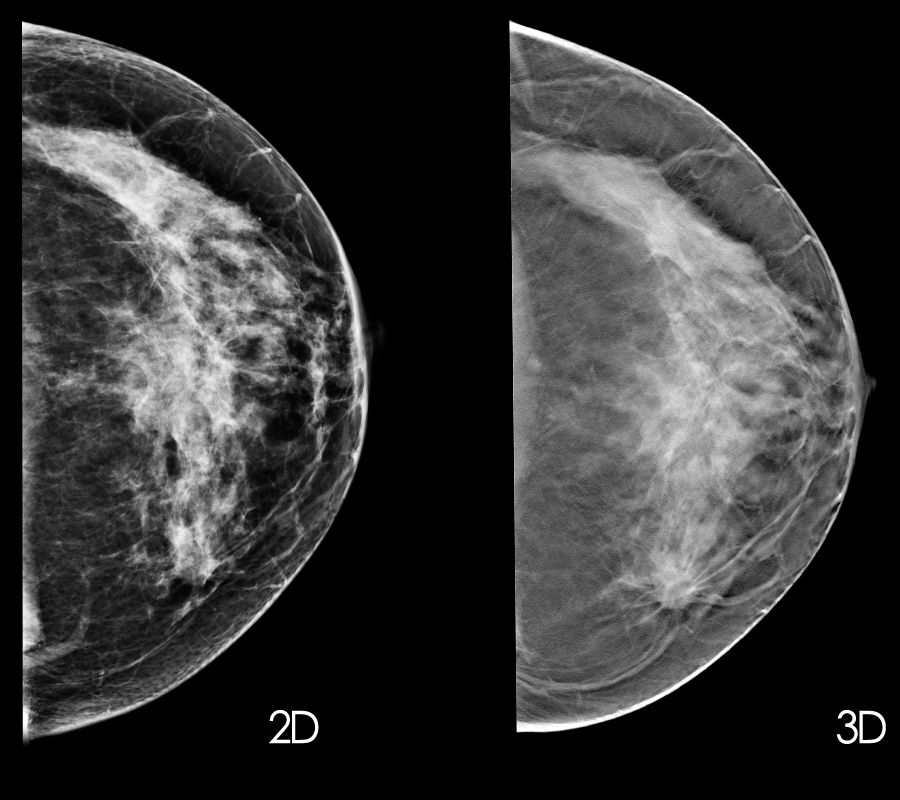
During a 3D mammogram, a potent x-ray “sweeps” over the breast, taking multiple images in a matter of seconds. These images are later displayed as “thin slices” that can be seen individually or in an interactive animation.
“Think of that stack of compressed breast tissue like a deck of playing cards. With the old mammograms, we are looking at the stack of compressed breast tissue at once, trying to determine if any bad cards are in there. Now with the 3D imaging, we are looking through that tissue, layer by layer. We can catch more tumors, particularly in dense breasts that could have been hiding in previous scans,” said Dr. Eva Duckett, director of breast imaging at Chesapeake Imaging Center.
Breast Cancer Awareness Month
The Breast Cancer Awareness Month was founded in October 1985, as a result of an agreement between the American Cancer Society and the now called AstraZeneca, which produces many anti-breast cancer drugs.
Evelyn Lauder, Senior Corporate Vice President of the Estée Lauder Companies, created The Breast Cancer Research Foundation a few years later in 1993. Lauder implemented the pink ribbon as the Foundation’s symbol, and from then on it became associated with breast cancer awareness.

Although many campaigns have brought awareness to breast cancer, many myths persist. One of the most common misconceptions regarding this disease is the thought that men cannot get breast cancer.
However, more than two thousand men are diagnosed with the disease in the United States each year, and around four hundred will die. Men carry a higher mortality rate than women as a consequence of this myth, which led them to seek treatment later.
Another widespread myth is believing that a mammogram can help breast cancer to spread. The compression of the breast tissue during the screening might be painful but is harmless. Finally, te majority of the women who get diagnosed with the disease have no family history of breast cancer.
The BRCA1 or BRCA2 genes
The genetic mutations BRCA1 and BRCA2 jumped to fame after actress Angelina Jolie underwent a mastectomy and got her ovarian removed after discovering she was a carrier. These genes increase the chances of developing breast cancer.
Women carrying the BRCA1 or BRCA2 genes have between 60 and 90 percent chance of developing breast or ovarian cancer, which is five times more than the average woman. There are plenty treatments if being diagnosed as a carrier, for example, undergoing a hormonal therapy called Tamoxifen.
Source: The Huffington Post
